The Development of Percutaneous Coronary Intervention
Percutaneous Coronary Intervention (PCI) is a minimally invasive procedure used to treat coronary artery stenosis or occlusion. Its development history can be traced back to the 1970s, and after years of technological advancements and innovations, PCI has become an important method in the treatment of cardiovascular diseases.
PCI development history
1. Initial stage (1970s)
In 1977, German doctor Andreas Gruentzig successfully performed the first percutaneous transluminal coronary angioplasty (PTCA), a technique that involves inserting a balloon into a narrowed coronary artery via a catheter and then inflating it to widen the vessel. This breakthrough opened new doors for the treatment of heart disease.
2. The Introduction of Stents (1980s)
In 1986, the first metal stent was applied in clinical settings, marking the entry of PCI into the stent era. Stents can maintain vascular patency after expansion, significantly reducing the risk of restenosis.
3. Drug-eluting stents (2000s)
To further reduce the incidence of restenosis, drug-eluting stents (DES) began to be widely used in 2003. This type of stent is coated with antiproliferative drugs on its surface, effectively inhibiting the proliferation of smooth muscle cells and reducing the probability of restenosis.
4. Technological Progress and Diversification (2010s to Present)
PCI technology continues to evolve, including new stent materials (such as biodegradable stents), more precise imaging technologies (such as optical coherence tomography OCT), and catheter techniques (such as finer catheters, ultrasound guidance, etc.). These innovations have improved the safety and effectiveness of interventional treatments.
5. Clinical Guidelines and Indication Expansion
As research deepens and technology advances, the indications for PCI have gradually expanded, from simple coronary artery stenosis to complex lesions (such as multivessel disease, left main disease, etc.), and in combination with drug therapy, forming a comprehensive treatment strategy.
The history of PCI is a journey of continuous innovation and improvement, with its notable efficacy and relatively low risk making it an important method in modern cardiovascular disease treatment. With the advancement of technology, PCI may continue to achieve breakthroughs in treatment outcomes and patient safety in the future.
coronary angiography
In the early days, selective coronary angiography was considered a taboo because it was generally believed that injecting contrast agent into the coronary arteries would inevitably lead to irreversible cardiac arrest. An accidental event became the trigger for breaking this taboo.
October 30, 1958
At the Cleveland Clinic in the United States, Mason Sones accidentally injected 30 ml of contrast agent into the right coronary artery while performing an aortic angiography on a patient with valve disease. Although the expected cardiac arrest occurred, the patient quickly returned to normal after coughing several times, which accelerated the expulsion of the contrast agent.
Sones speculated that the coronary arteries might be able to tolerate a small amount of direct contrast agent injection, and subsequent extensive basic and clinical studies confirmed Sones' inference. Immediately following, selective coronary angiography gradually developed, becoming a milestone in the history of coronary heart disease diagnosis and treatment.
1959-1967
In 1959, pediatric cardiologist Mason Sones and others at the Cleveland Clinic performed the first selective coronary angiography.
In 1966, Amplatz and in 1967, Judkins further improved the catheter tip shape, curvature, and catheter insertion techniques, leading to the widespread application of selective coronary angiography.
coronary intervention development
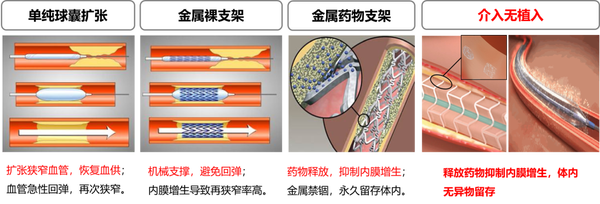
Coronary intervention has gone through the eras of plain balloon angioplasty, bare metal stents, and drug-eluting metal stents, and has now entered the era of bioresorbable stents and drug-coated balloons.
Percutaneous Transluminal Coronary Angioplasty (PTCA)
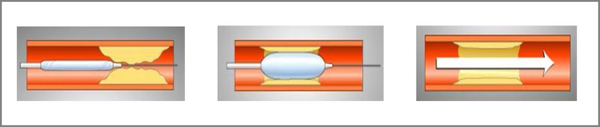
Percutaneous Coronary Angioplasty (Percutaneous Coronary Angioplasty, PTCA) The term PTCA broadly covers all interventional treatment methods for coronary heart disease, but in a narrow sense, it often refers to the traditional coronary balloon angioplasty (i.e., POBA, short for Plain old balloon angioplasty). Using the femoral artery approach or the radial artery approach, the guiding catheter is delivered to the opening of the coronary artery to be dilated, and then a balloon of the corresponding size is sent along the guide wire to the narrowed segment. According to the characteristics of the lesion, it is expanded with appropriate pressure and time to achieve the purpose of relieving stenosis.
In 1964, America's Dotter successfully used a homemade balloon catheter to treat a patient with severe femoral artery occlusion and achieved complete success.
Since 1974, Andreas Gruentzig from Germany began to study the application of balloon technology to coronary arteries, but his colleagues and teachers around him criticized his idea as unscientific. Even after successfully experimenting on dog coronary arteries, many people still mocked him as mentally abnormal. However, Gruentzig did not lose heart and persisted in his research direction.
In 1977, Gruentzig boldly drew on peripheral intervention techniques to complete the world's first percutaneous coronary angioplasty, achieving a minimally invasive approach to treating coronary heart disease and pioneering modern interventional cardiology. By 1985, Gruentzig alone had performed 2,623 PTCA procedures, with a success rate of over 90%, and only 2 deaths.
The main issues of PTCA:
-
plaque rupture and collapse risk
-
acute occlusion rate 2-12%
-
restenosis rate as high as 30-50%
2. Coronary stent implantation
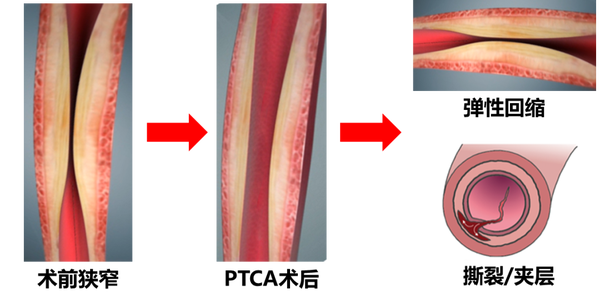
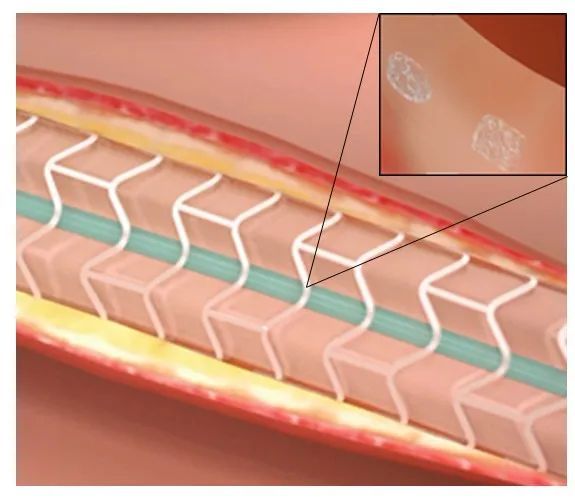
Placing a mesh-like stent made of materials such as stainless steel with gaps into the narrowed segments of the coronary artery to support the vessel wall and maintain blood flow, which can reduce vascular elastic recoil after PTCA and seal any dissections that may occur during PTCA, greatly reducing the incidence of acute vessel occlusion during the procedure.
3. Bare Metal Stent (BMS)
In 1986, Urich Sigwart first used the bare metal stent (BMS) in humans, providing permanent intravascular mechanical support, and it became the first FDA-approved stent.
-
effective blocking of the interlayer, basically solving acute and subacute occlusion issues
-
解决了血管壁弹性回缩问题,再狭窄率有所下降 Solved the issue of vascular wall elastic recoil, and the restenosis rate has decreased
limitations of BMS:
-
The stress stimulation produced by the stent on the vascular endothelium accelerates the proliferation of endothelial cells, leading to restenosis. Relevant studies have pointed out that the restenosis rate of BMS is as high as 20%-30%.
-
Restenosis is caused by factors such as vascular elastic recoil, negative remodeling, thrombosis at the injured site, proliferation and migration of smooth muscle cells, and excessive proliferation of extracellular matrix. In-stent restenosis of BMS is mainly due to the excessive proliferation of smooth muscle cells.
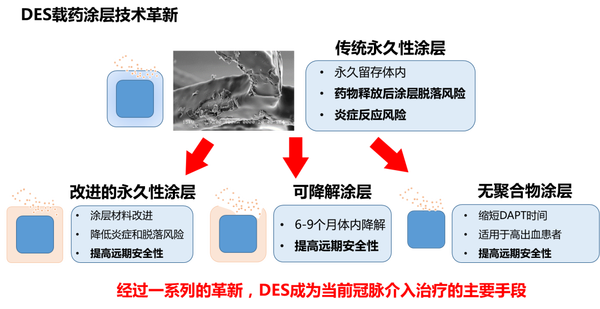
4. Metal drug-eluting stent (DES)
Drug-eluting stents control the release of certain antiproliferative drugs through a specific carrier on the surface of the stent, inhibiting excessive proliferation of the vascular intima after stent surgery by continuous action with the vessel wall, thereby reducing the incidence of restenosis.
In September 2001, the famous RAVEL trial results were announced at the European Society of Cardiology in Sweden. The RAVEL trial showed that compared with bare-metal stents, the 7-month restenosis rate for the Sirolimus-eluting stent (SES) group was 0. In December of the same year, drug-eluting stents topped the AHA's Top Ten Research Advances of the year.
In recent years, with the application of DES in PCI procedures, clinical trials and studies have shown that it has unique application value in preventing restenosis. This is because, on one hand, it can reduce coronary artery elastic recoil after balloon expansion, and on the other hand, it can provide slow and long-term high-concentration drug release to the local coronary lesion, inhibiting excessive cell proliferation, thereby effectively reducing the restenosis rate.
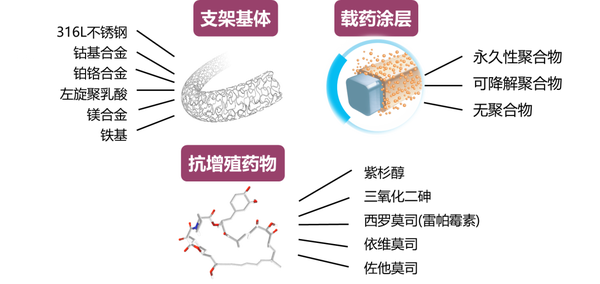
DES is mainly composed of stent substrate, antiproliferative drug, and drug-loading coating, which allows for the optimization of stent technology.
support structure
closed-loop structure

Advantages:
Strong support, can well cover the lesion area plaque
shortcomings
-
stent deliverability is poor
-
unable to obtain a larger side port area
-
High metal coverage can cause greater irritation to the vessel wall, making it easier for thrombosis to occur.
-
The smaller and more regular distribution of the support angles between the supporting structures can enable the stent to withstand higher shear forces, and when the shear force it bears exceeds its compliance, the stent is prone to fracture.
open-loop structure

Advantages:
-
The stent has better flexibility and is easier to pass through tortuous lesions.
-
Improve the axial flexibility of the stent and reduce the amount of axial shortening
-
larger side opening area, easy to handle branch lesions
shortcomings
-
not conducive to the even distribution of drugs on the vascular wall
-
support force weaker than closed-loop stent
medication
Rapamycin
-
inhibiting the progression from G1 to S phase in the smooth muscle cell cycle, thereby inhibiting proliferation
-
The efficacy of inhibiting in-stent restenosis is stronger than that of paclitaxel.
-
Within the clinical therapeutic dose range, no apoptosis of smooth muscle cells occurred, thus the effective dose range is relatively broad.
-
The diffusion coefficient of rapamycin in the vessel wall is twice as high as that of paclitaxel.
Paclitaxel
-
Acts on microtubules during the G2 and M phases of cell division, inhibits smooth muscle cell mitosis, causing cell apoptosis
-
Advantages: strong liposolubility, easily and quickly absorbed by tissues
-
Disadvantages: cytotoxic effects
Everolimus
-
rapamycin derivatives
-
inhibiting smooth muscle cell proliferation more effectively than rapamycin
Zotarolimus
-
effectively inhibit restenosis occurrence
-
Compared to sirolimus, its pharmacokinetics are superior
Arsenic trioxide
-
short-term suppression of rapid endothelial cell proliferation
-
Long-term auxiliary stent integration into the inner layer of the vessel, covered by endothelial cells to achieve stable endothelialization
biodegradable stent (BRS)
biodegradable stent, refers to:
-
Made of a type of material (polymeric materials, magnesium, zinc, iron, etc.) that can be degraded and absorbed in the human body;
-
Stent carries drugs, resisting vascular restenosis through drug slow release;
-
ultimately degrading and being completely absorbed by the tissue, with vascular structure and function restored.
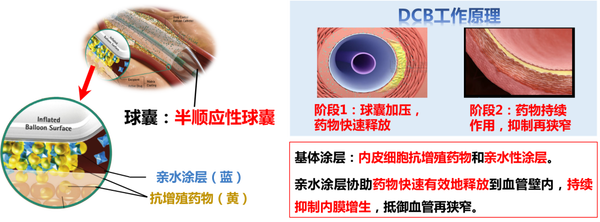
drug-eluting balloon (DCB)
Drug balloons typically use semi-compliant balloons as drug delivery devices, with the balloon surface coated with antiproliferative drugs for endothelial cells and a hydrophilic coating. The hydrophilic coating assists in the rapid and effective release of the drug into the vessel wall, continuously inhibiting intimal hyperplasia and resisting vascular restenosis. Advantages: Avoids the risks and drawbacks of permanent implants, provides more uniform drug distribution, and shortens the postoperative dual antiplatelet therapy duration.
5. Summary
The PTCA balloon dilation era, which began in 1977, opened the way for coronary intervention, but due to the high acute recoil rate of blood vessels, the effect of vessel opening was poor, with a restenosis rate as high as about 50%, urgently requiring long-term vascular support. After a series of research and development and clinical studies, bare metal stents with permanent support were created, avoiding the acute recoil of blood vessels. However, due to the excessive proliferation of smooth muscle cells during the repair process, the restenosis rate of metal stents still remained at 20%-30%.
On the basis of bare metal stents, to inhibit the excessive proliferation of smooth muscle cells leading to restenosis, drug-eluting metal stents were developed. The birth of drug-eluting metal stents reduced the restenosis rate to below 5%. Although drug-eluting metal stents perfectly solved the problem of restenosis, late thrombosis, vascular inflammation, late catch-up, and the weakening of the vessel wall's motility function became important reasons limiting the development of drug-eluting metal stents. To improve prognosis, bioresorbable scaffolds and drug-coated balloons emerged.
【Copyright and Disclaimer】The above information is collected and organized by PlastMatch. The copyright belongs to the original author. This article is reprinted for the purpose of providing more information, and it does not imply that PlastMatch endorses the views expressed in the article or guarantees its accuracy. If there are any errors in the source attribution or if your legitimate rights have been infringed, please contact us, and we will promptly correct or remove the content. If other media, websites, or individuals use the aforementioned content, they must clearly indicate the original source and origin of the work and assume legal responsibility on their own.
Most Popular
-

Key Players: The 10 Most Critical Publicly Listed Companies in Solid-State Battery Raw Materials
-

Vioneo Abandons €1.5 Billion Antwerp Project, First Commercial Green Polyolefin Plant Relocates to China
-

EU Changes ELV Regulation Again: Recycled Plastic Content Dispute and Exclusion of Bio-Based Plastics
-

Clariant's CATOFIN™ Catalyst and CLARITY™ Platform Drive Dual-Engine Performance
-

List Released! Mexico Announces 50% Tariff On 1,371 China Product Categories






